Topics
1.1.1 Anatomy of a Normal Breast
1.1.2 Risk Factors of Breast Cancer
1.1.3 Breast Density
1.1.4 Gene Mutations
1.1.5 Significance
Chapter 1: Learning Activity
Learning Objectives
➤ Explain the anatomy of a normal breast.
➤ Illustrate the risk factors of breast cancer.
➤ Define breast density.
➤ List gene mutations related to breast cancer.
1.1.1 Anatomy of a Normal Breast
Breasts are composed of three different types of tissue, collectively known as breast tissue: fibrous, glandular, and fatty (Centers for Disease Control and Prevention [CDC], 2022a). Fibrous tissue is the structure that holds the breast together and in place; meanwhile, the glandular tissue is where the lobules and ducts live. Together these two tissues are known as fibroglandular tissue. Fatty tissue fills in whatever space remains in the breast.
Behind your breast tissue is a layer of muscle (pectoral or chest muscle) and various bones (Lymphedema Working Group, 2012).
Breast tissue is not limited to the breast itself; it also covers most of your chest, including the area from your armpits to your collarbone to your breastbone (Canadian Breast Cancer Network [CBCN], 2022). Various blood and lymph vessels in your breast tissue help fight infections and viruses and remove bacteria and cancer cells.
The vital features of the breasts milk production are the lobules and ducts mentioned above. Lobules produce the milk, while the duct vessels transport the milk to the nipple (Lymphedema Working Group, 2012).
See Image 3 for a detailed diagram of the breast (Lynch & Morgoth666, 2015).
Image 3: Normal breast anatomy cross-section
Legend
1. Chest wall, 2. Pectoralis muscles, 3. Lobules, 4. Nipple surface, 5. Areola, 6. Lactiferous duct, 7. Fatty tissues, 8. Skin.
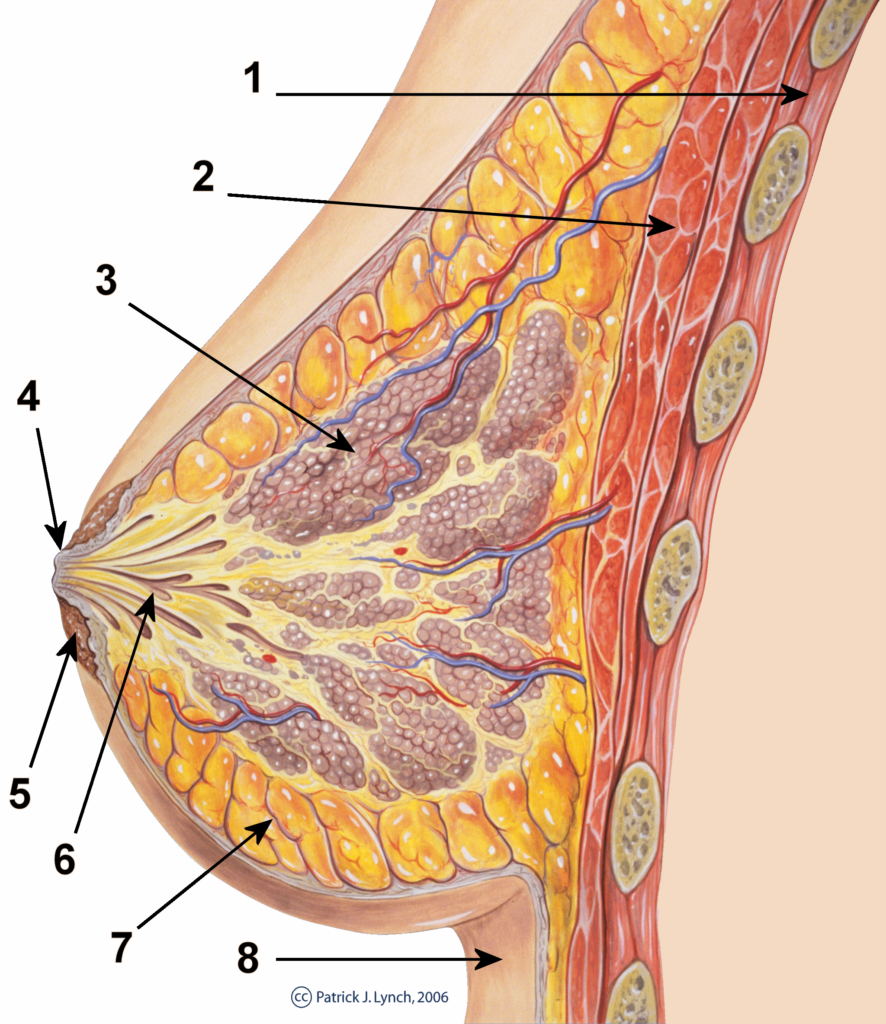
(Patrick J. Lynch and Morgoth666 / Wikimedia Commons)
CC BY
1.1.2 Risk Factors of Breast Cancer
Specific characteristics can increase your chances of developing breast cancer. You may or may not be able to change these risk factors (CBCN, 2022).
The Canadian Breast Cancer Network (2022) highlights the following modifiable factors:
- smoking,
- increased alcohol intake,
- obesity,
- no pregnancy,
- first pregnancy after age 30,
- hormone replacement therapy (for over two years of combined hormones, or over 10 years of estrogen alone),
- some previous fertility therapy hormones,
- not having breast fed,
- high-fat diet,
- high socio-economic status,
- physical activity,
- exposure to ionizing radiation,
- and oral contraceptives (CBCN, 2022).
Furthermore, the CBCN lists the following as non-modifiable factors:
- age,
- family history of breast cancer (also in men),
- family history of some other cancers (e.g., uterine, ovarian),
- starting menstruations early (before age 12),
- reaching menopause late (after age 55),
- previous biopsy showing abnormal breast cells,
- dense breast tissue,
- and inherited mutations (e.g., BRCA1, BRCA2) (CBCN, 2022).
If you would like to learn more about reducing your risk of breast cancer, check out Video 1 (CDC, 2018).
Video 1
How Can I Reduce My Risk of Breast Cancer? (CDC, 2018)
1.1.3 Breast Density
Breast density refers to the amount of fibroglandular tissue compared to fatty tissue (CDC, 2022b). The type of test to determine breast density is called a mammogram.
Many medical centres use the American College of Radiologist Breast Imaging Reporting and Data System (BI-RADS) to categorize breast density into one of four categories:
- BI-RADS A — Mostly fatty tissue.
- BI-RADS B — Few areas of dense fibrous and glandular tissue.
- BI-RADS C — Equal amount of dense tissue and fatty tissue.
- BI-RADS D — Entire breasts contain dense tissue. (CBCN, 2022)
The first two categories are classified as “low-density, non-dense, or fatty breasts,” while the latter two are “high-density or dense breasts” (CDC, 2022b).
Breast density can affect your risk of developing breast cancer (CDC, 2022b). Scientists have found that having denser breasts increases the risk of breast cancer; however, they are unsure why that is the case.
According to the CDC, dense breasts are more common in individuals who:
- are younger,
- are pregnant or breastfeeding,
- are taking hormone replacement therapy,
- and have a lower body weight (CDC, 2022b).
For more information on breast density, check out Video 2 (ScreeningBC, 2020).
Video 2
Breast Density and Screening Mammograms (English)
Also available in French, Punjabi, Mandarin, and Cantonese (ScreeningBC, 2020)
1.1.4 Gene Mutations
Genes can play a significant role in breast cancer development (CBCN, 2022). These genes usually mutate to either increase the likelihood of developing breast cancer or affect how fast existing tumours grow. Some of these genes are hereditary, while others mutate during your lifetime.
Sub-Types of Breast Cancer
Breast cancer has sub-types that depend on whether certain receptors are present on the cancer cells.
Hormone receptor-positive (HR+) breast cancer refers to cancers in which the cells have receptors that can receive signals from hormones that drive cell growth (CBCN, n.d.b).
Human epidermal growth factor receptor 2 (HER2) is a gene that controls how many HER2 receptors are available on a cell’s surface (CBCN, 2022). While normal cells only have two copies of this gene, cancer cells in around 15% of breast cancers contain more than two copies. This type of breast cancer is called HER2 positive. Because of the overexpression of HER2, this HER2-positive breast cancer can spread much faster than usual and, therefore, requires specialized treatment.
Triple-negative breast cancer refers to cancers whose growth is not driven by the hormones estrogen or progesterone or by the overexpression of HER2 proteins (CBCN, n.d.c).
Check out the following resource for more information on breast cancer types and sub-types:
Types & Sub-Types (CBCN, n.d.b)
Hereditary Genes
Certain gene mutations inherited from your parents can increase your chance of developing breast cancer (CBCN, 2022). The breast cancer gene (BRCA) is the most common one.
BRCA1 and BRCA2 are tumour-suppressor genes that help prevent uncontrollable cancer growth (CBCN, 2022). When a mutation occurs in this gene, it is unable to suppress tumours as effectively, which may lead to breast cancer development.
Other less common hereditary gene mutations are CHEK2 and PALB2 (Canadian Cancer Society, n.d.9). CHEK2 is a tumour-suppressor gene, while PALB2 helps repair DNA, similar to BRCA. Mutations in either one increase your risk of developing breast cancer.
1.1.5 Significance
Certain population groups are more likely to be carriers of the hereditary genes mentioned above (CBCN, 2022). For example, people with Ashkenazi Jewish ancestry are more likely to be carriers of BRCA1 and BRCA2.
As mentioned previously, there are ways to prevent or decrease your risk of developing breast cancer.
Chapter 1: Learning Activity
Click on the (+) to reveal each part of the breast anatomy.
Image 3: Breast anatomy normal scheme
(Patrick J. Lynch and Morgoth666 / Wikimedia Commons)
CC BY