Topics
2.2.1 Treatment Plan
2.2.2 Breast-Conserving Surgery
2.2.3 Lumpectomy
2.2.4 Mastectomy
2.2.5 Total Mastectomy
2.2.6 Modified Radical Mastectomy and Radical Mastectomy
2.2.7 Prophylactic Mastectomy
2.2.8 Lymph Node Removal
2.2.9 Surgery Questions to Ask
Learning Objectives
➤ List the parts of a treatment plan.
➤ Explain what breast-conserving surgeries are.
➤ Compare the different types of breast-conserving surgeries.
➤ Explain the purpose of a prophylactic mastectomy.
➤ Explain the purpose of lymph node removal.
2.2.1 Treatment Plan
As mentioned previously, there are various factors to consider when creating your personal treatment plan, such as:
- lifestyle,
- spiritual, religious, and cultural beliefs,
- and stage of life.
Open and honest communications with your healthcare team allows them to create a treatment plan that best suits your needs.
Your Healthcare Team
Your healthcare team is an important part of your treatment plan. This team can be made up of a variety of individuals, including:
- family physicians,
- surgical oncologists,
- radiation oncologists,
- oncology nurses,
- registered nurses,
- licensed practical nurses,
- registered social workers,
- registered dietitians,
- complementary and alternative therapy members,
- radiation therapists,
- diagnostic technicians (X-ray, ultrasound, MRI, PET, etc.) (Lymphedema Working Group, 2012).
2.2.2 Breast-Conserving Surgery
Breast-conserving surgery involves removing the tumour in your breast(s) and some tissue in the surrounding area (Lymphedema Working Group, 2012). The goal of this type of surgery is to remove the cancer while saving as much of the breast(s) as possible. There are various types of breast-conserving surgery, but the most common is a lumpectomy.
Sometimes, breast-conserving surgery is not appropriate for your stage of breast cancer (Lymphedema Working Group, 2012). For example, if there are multiple tumours in your breast(s), then your healthcare team might suggest a mastectomy instead. You may want to talk with your healthcare provider, family practitioner, or oncologist if you are pregnant or have an autoimmune disease, such as lupus.
Additionally, you should not have radiation therapy if you have certain health conditions, including pregnancy and some autoimmune diseases (e.g., lupus).
As mentioned previously, make sure that you consider your lifestyle before adding radiation to your treatment plan (Lymphedema Working Group, 2012). Radiation therapy requires a daily commitment that may not work for you.
2.2.3 Lumpectomy
A lumpectomy involves removing the tumour and some of the surrounding tissue (Lymphedema Working Group, 2012). This procedure is an option if the tumour is less than 4 cm in size and has clear, defined margins. Radiation therapy right after a lumpectomy ensures the elimination of the cancer.
See Image 10 for a graphic illustration of surgery of a segmental mastectomy or lumpectomy (Bartlett & National Cancer Institute, 2013).
Image 10
Surgery of a segmental mastectomy or lumpectomy
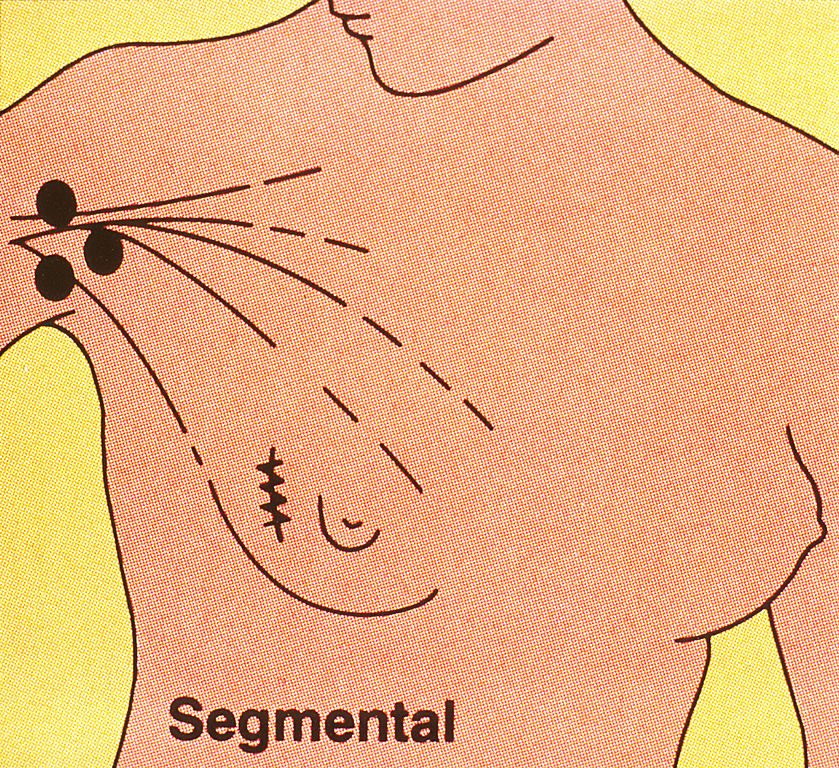
(Linda Bartlett and National Cancer Institute / Wikimedia Commons)
PDM
2.2.4 Mastectomy
If breast-conserving surgery with radiation therapy is not feasible or wanted, a mastectomy is recommended (Lymphedema Working Group, 2012). Mastectomies may require radiation therapy afterward.
Things to consider when having a mastectomy are what type of mastectomy you will be having, how long your hospital stay might be, and what follow-up care is required (Canadian Breast Cancer Network [CBCN], 2022).
This chapter will discuss three mastectomy types: total, modified radical, and prophylactic (Lymphedema Working Group, 2012).
2.2.5 Total Mastectomy
A total mastectomy involves removing the whole breast, nipple, and some of the surrounding tissue; however, the chest muscles, nearby lymph nodes, and nerves remain intact (Lymphedema Working Group, 2012).
Your healthcare team might suggest a total mastectomy if your tumour is large, you have multiple tumours in your breast(s), or radiation is not feasible (Johns Hopkins Medicine, n.d.b).
Having a total mastectomy eliminates the possibility of breast cancer reoccurring (Lymphedema Working Group, 2012).
See Image 11 for a total mastectomy, which illustrates the parts of the breast tissue to remove (National Cancer Institute, 2013).
Image 11
Total mastectomy
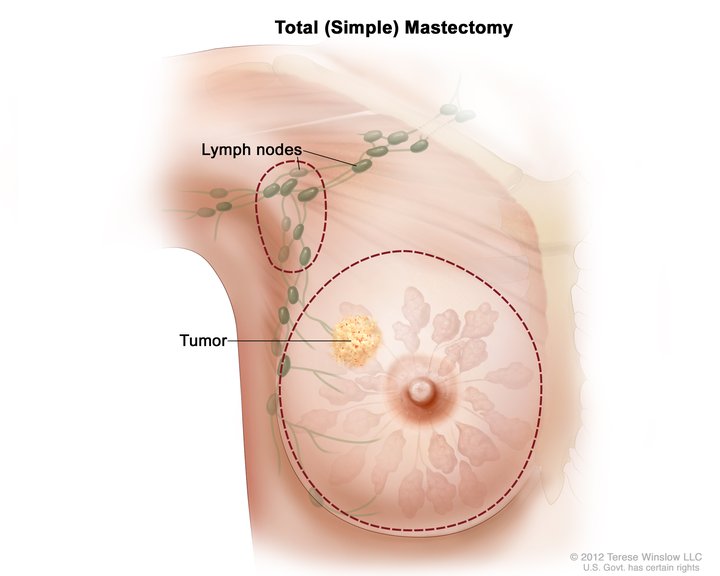
(National Cancer Institute / Wikimedia Commons)
PDM
2.2.6 Radical Mastectomy & Modified Radical Mastectomy
Similar to a total mastectomy, a radical mastectomy removes the whole breast, nipple, and some of the surrounding tissue (CBCN, 2022). The difference is it also removes some lymph nodes under the arm, some nerves, and the chest muscles.
Side effects of a radical mastectomy include pain, swelling, and weakness in the side you had surgery on (CBCN, 2022).
See Image 12 for an illustration of a radical mastectomy (Bartlett & National Cancer Institute, 2013b).
Image 12
Radical mastectomy
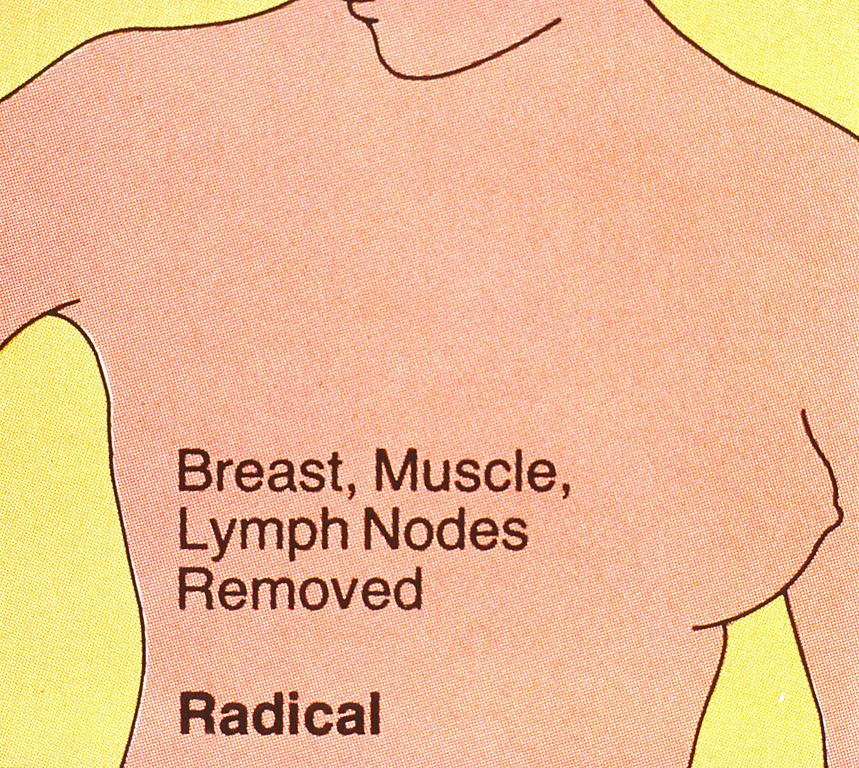
(Linda Bartlett and National Cancer Institute / Wikimedia Commons)
PDM
Although radical mastectomies used to be the standard surgical treatment, nowadays, it is rarely performed unless the cancer has spread to the chest muscles (Johns Hopkins Medicine, n.d.b).
Instead, you can have a modified radical mastectomy done. A modified radical mastectomy is identical to a radical mastectomy, except it preserves the chest muscles and nerves. (CBCN, 2022). Side effects of this procedure are similar to a radical mastectomy, but they are less severe.
Your healthcare team might recommend a modified radical mastectomy if you have invasive breast cancer (Lymphedema Working Group, 2012).
See Image 13 for an illustration of a modified radical mastectomy (National Institutes of Health, 2020).
Image 13
Modified radical & radical mastectomies

cancer treatment – a guide for patients (1998)
(National Institutes of Health / Wikimedia Commons)
PDM
2.2.7 Prophylactic Mastectomy
A prophylactic mastectomy is a form of breast cancer prevention rather than treatment (Lymphedema Working Group, 2012). You might choose to have a prophylactic mastectomy if you have numerous breast cancer risk factors. These risk factors can include the BRCA1 and BRCA2 genes, a family history of breast cancer, or a previous breast cancer diagnosis.
You should be aware of the risks of this type of surgery. Make sure to talk to your healthcare team about the risks and benefits of a prophylactic mastectomy.
Hereditary Breast Cancer
Hereditary breast cancer is an “autosomal dominant cancer susceptibility syndrome, most commonly associated with an inherited BRCA1 or BRCA2 gene mutation” (BC Cancer, 2018). Other high-risk genes include PALB2, TP53, PTEN, STK11, CDH1.
Check out the following resources for more information:
Inherited Mutations (Facing Our Risk of Cancer Empowered, 2024).
Hereditary Cancer (BC Cancer, n.d.w).
2.2.8 Lymph Node Removal
Your healthcare team might recommend a lymph node removal procedure (Lymphedema Working Group, 2012). Lymph nodes are parts of your body that filter abnormal cells, bodily fluids, and dead cells. A common area for lymph node removal with breast cancer is the armpit.
There are two types of lymph node removal: axillary lymph node dissection and sentinel lymph node biopsy (Lymphedema Working Group, 2012). An axillary lymph node dissection involves removing the lymph nodes in the armpit. Examining the removed lymph nodes will determine if the cancer has spread. Meanwhile, a sentinel lymph node biopsy only removes the lymph nodes that may be filtering cancer cells from the breast. If the lymph nodes contain cancer, you may have more of them removed.
Both types of lymph node removal might cause side effects such as pain, limited arm movement on the side the surgery was on, and lymphedema (swelling in the arm) (CBCN, 2022). However, a sentinel lymph node removal causes less severe side effects.
After lymph node removal is complete, a drain will be left in the incision site to help remove any fluids that gather there (CBCN, 2022).
For more information about surgery for breast cancer, check out the following resource:
Surgery Choices for Women with DCIS or Breast Cancer (National Cancer Institute, 2022b).
2.2.9 Questions to Ask About Surgery
- With my specific cancer diagnosis, is there one type of surgery that is more successful than others?
- What will I be able to do after surgery?
- Will I be in the hospital for a long time after my surgery? If I need to stay in the hospital, how long will I need to stay?
- What types of mastectomies I’m eligible for?
- What are the side effects and the risks of the surgery that I am going to be receiving?
- Am I a good candidate for breast-conserving surgery?
- Am I able to receive breast reconstruction surgery during my tumour removal surgery?
- Will you provide information on what I should watch for after my surgery?
- I am feeling anxious about receiving this surgery; do I have time to think about what I want to do?
- Will I need rehabilitation support? Where do I look for resources for rehabilitation support? (Lymphedema Working Group, 2012)