Topics
1.2.1 What is Screening?
1.2.2 Breast Self-Examination
1.2.3 Clinical Breast Examination
1.2.4 Who Should Get Screened for Breast Cancer
Learning Objectives
➤ Explain what screening is
➤ Explain how to self-examine breasts
➤ Explain what happens during a clinical breast examination
1.2.1 What is Screening?
Screening is the process of checking for signs of a disease, such as breast cancer, when no symptoms are shown (Canadian Cancer Society, n.d.10). This process helps catch breast cancer early to improve your chances of recovery. You can be screened for breast cancer by yourself or your physician.
All the provinces and territories in Canada have different screening programs for breast cancer (Canadian Breast Cancer Network [CBCN], 2022). Because of this, you need to understand how the breast cancer screening process works in your province or territory.
1.2.2 Breast Self-Examination
Breast self-examinations check for any lumps or changes in your breasts (Healthwise Staff, 2022). You should complete these examinations every month, preferably one week after you begin to menstruate. Examining your breasts at the same time every month can make it easier to identify if there are any noticeable changes. However, if your menstruation cycle is irregular or you don’t menstruate, then you can pick a day of the month that is easy to remember.
Here are the steps to complete a breast self-examination:
- Start by removing any clothes covering your breasts.
- There are two different positions you can take, so pick the one that is more comfortable for you:
- Laying down — causes your breasts to become even, which allows you to feel lumps more easily.
- Standing — stand in the shower or in front of a mirror.
- Examine all of your breast tissue, which ranges from your collarbone to your breastbone to your armpits to the bottom of your bra line.
- Instead of using your fingertips, use the pads of your three middle fingers on the opposite hand to the breast you are examining (e.g., right middle fingers for the left breast).
- Slowly move your fingers in small coin-sized circles in the areas mentioned in Step 3.
- There are three levels of pressure you should use:
- Light pressure — for feeling the tissue closest to your skin’s surface
- Medium pressure — for feeling the tissue a little deeper
- Firm pressure — for feeling the tissue around your breastbone and ribs
- Keep your fingers on your skin for the duration of the examination. (Healthwise Staff, 2022)
See Image 4 for a visual example of a breast self-examination (National Cancer Institute, 2008).
Image 4: Breast self-examination visuals
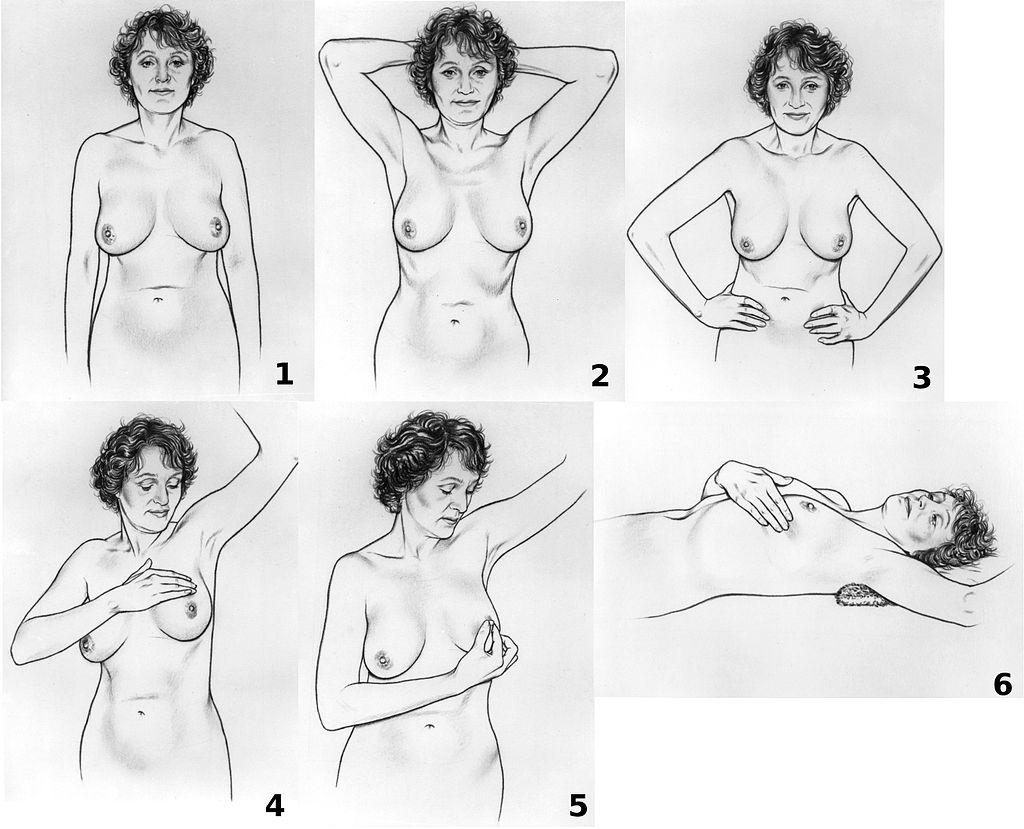
(National Cancer Institute / Wikimedia Commons)
PDM
For more information on breast self-examinations, check out Video 3 (BBC News, 2021) and Video 4 (Screening BC, 2018).
Video 3
How to do a breast cancer self-examination – BBC News (BBC News, 2021)
Video 4
BC Cancer – Johnna’s Snippet – Breast Screening (Screening BC, 2018a)
1.2.3 Clinical Breast Examination
If you notice a change in your breast(s) through your self-examination, you might have a clinical breast examination done (Canadian Cancer Society, n.d.i). You could also have this examination as part of your routine check-up with your healthcare provider.
Here are the steps for a clinical breast examination, according to the Canadian Cancer Society (n.d.i):
- Your healthcare provider will ask you to remove any clothing covering your breasts.
- Your healthcare provider will then examine your breasts visually for any abnormalities, including:
- changes or differences in breast shape
- fullness or thickness in one breast, but not the other
- changes in skin colour, temperature, and texture (e.g., dimpling, redness, or increased warmth)
- rashes
- lumps or swelling
- discharge from the nipple
- nipple changes (e.g., inverting).
- Next, your healthcare provider will ask you to lie down so they can physically examine your breasts.
- Your healthcare provider will apply firm pressure with their fingers to examine your breast tissue and look for abnormalities, including:
- lumps
- hardening or thickening
- tenderness or pain
- Your healthcare provider will let you know if they find any abnormalities and discuss if further testing is required. (Canadian Cancer Society, n.d.i)
1.2.4 Who Should Get Screened for Breast Cancer
BC Cancer (2018) recommends that women should receive annual breast cancer screening if they are over 40 and have someone in their immediate family with breast cancer. If they do not have an immediate family member with breast cancer, then they should be screened every two years.
Low Screening Rate Groups
However, some population groups that fit the above criteria are less likely to be screened for breast cancer (BC Cancer, 2018b). For example, people who have immigrated to BC from Eastern Europe, Central Asia, and certain other Asian countries had lower screening rates than other immigrant groups. These Asian countries include Korea (39%), China (45.7%), India (44.5%), and the Philippines (45.9%). These screening rates are lower than the ones for people already living in British Columbia (50.3%).
One factor that can affect the likelihood of receiving breast cancer screening is whether or not the person has a family physician (BC Cancer, 2018b). People with a family doctor were more likely to receive screening than those without one.